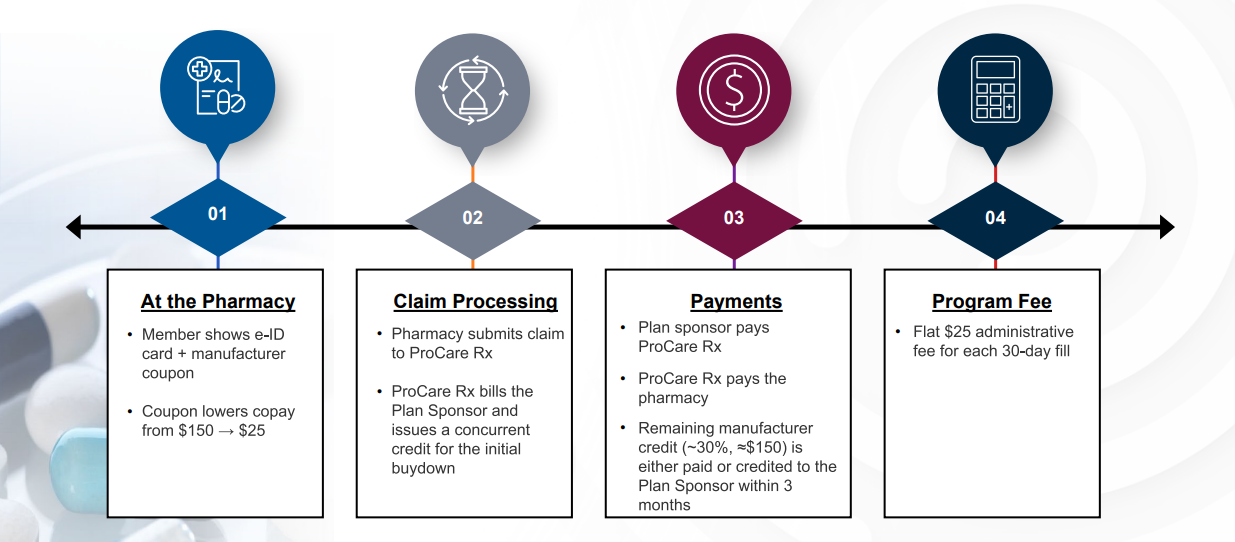
How It Works
ProCare Rx’s Zepbound® Program reduces member out-of-pocket costs while maintaining full transparency for plan sponsors. Members present their digital ID and manufacturer coupon at the pharmacy, lowering their copay at the point of sale. ProCare Rx processes the claim, applies the manufacturer credit, and coordinates payment with the pharmacy. The plan sponsor receives the remaining manufacturer credit, with a simple flat administrative fee applied per fill.